What Is Dialysis Access?
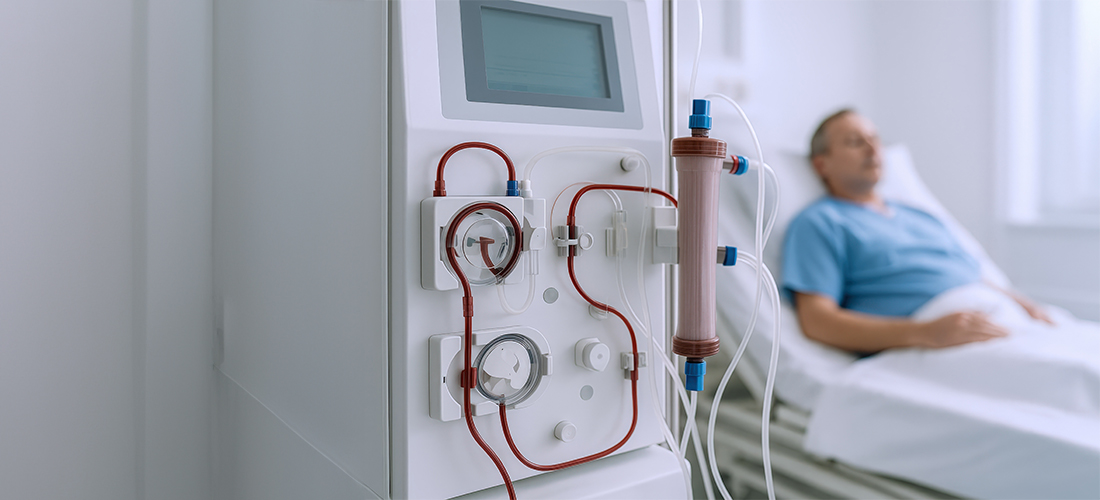
Dialysis access is a surgically created pathway that allows blood to flow between your body and the dialysis machine at a high, steady rate. It is designed to handle large volumes of blood, withstand repeated needle insertions, and remain reliable over long periods. Most dialysis access sites are created in the arm, though the exact location depends on your blood vessels and overall health.
Understanding dialysis access empowers patients to protect it, recognise problems early, and work confidently with the care team.
Why Do I Need Dialysis Access?
Healthy kidneys remove waste products, excess fluid, and toxins from the blood. When kidneys fail, dialysis takes over this function.
During hemodialysis, blood must leave your body, be cleaned by a dialysis machine, and return safely to your circulation. To do this efficiently and repeatedly, a special access point is required.
Why Can't Regular Veins Be Used?
Regular veins are too small, have slower blood flow, and can collapse or become damaged easily. Dialysis requires strong vessels with high, continuous blood flow and repeated access several times a week. Dialysis access is specially designed to meet these demands safely and consistently.
Without a reliable access:
- Dialysis cannot be performed effectively
- Treatments may be interrupted
- The risk of complications increases
Important Terminology You Should Know
Thrill
A gentle vibration felt when you place your fingers lightly over your fistula or graft. Indicates that blood is flowing properly and should be present at all times. Check for the thrill daily. If it suddenly disappears or becomes very weak, seek urgent medical attention.
Bruit
A whooshing sound heard over the access when a healthcare provider listens with a stethoscope. Confirms blood flow through the access.
Maturation
The process by which a fistula becomes strong and large enough to be used for dialysis (typically 4–6 weeks or longer).
Cannulation
The process of inserting dialysis needles into a fistula or graft to start hemodialysis.
Stenosis
A narrowing of the blood vessel within the access that reduces blood flow.
Thrombosis
A blood clot that blocks the access and prevents dialysis from being performed.
Aneurysm
An abnormal bulging or widening of the blood vessel, usually caused by repeated needle punctures.
Duplex Ultrasound
A non-invasive imaging test that uses sound waves to assess blood flow and access structure.
Types of Dialysis Access
There are three main types of dialysis access. Your nephrologist and vascular specialist will help determine which is best for you.
1. Arteriovenous (AV) Fistula — The Gold Standard
An AV fistula is created by directly connecting an artery to a vein, usually in the forearm or upper arm. Over time, the vein becomes larger and stronger due to increased blood flow.
Advantages:
- Longest-lasting access
- Lowest risk of infection
- Best blood flow for dialysis
Limitations:
- Takes time to mature (usually 4–8 weeks or longer)
- Not all patients have suitable veins
2. Arteriovenous (AV) Graft
If natural veins are not suitable for a fistula, an AV graft may be used. This involves placing a soft synthetic tube to connect an artery and a vein.
Advantages:
- Can be used sooner than a fistula (usually within 2–3 weeks)
- Suitable for patients with smaller or weaker veins
Limitations:
- Higher risk of infection than a fistula
- More prone to narrowing and clotting over time
3. Dialysis Catheter (Central Venous Catheter)
A dialysis catheter is a tube placed into a large vein, usually in the neck or chest.
Used for:
- Emergency dialysis
- Short-term access while a fistula or graft matures
Limitations:
- Highest risk of infection
- Lower blood flow
- Can damage veins over time
Important: Catheters are not recommended for long-term dialysis whenever alternatives are available. They are associated with bloodstream infections, clotting, and narrowing of major veins.
When Should Dialysis Access Be Created?
Dialysis access should ideally be created before dialysis becomes urgently necessary.
Early planning allows:
- Time for healing and maturation
- Reduced reliance on temporary catheters
- Better long-term outcomes
Your nephrologist will usually refer you for access planning when kidney function declines significantly, even if dialysis has not yet started.
When Can My Access Be Used?
- AV Fistula: Typically 4–6 weeks after surgery, once mature
- AV Graft: Usually 2–3 weeks after placement
- Catheter: Can be used immediately
Daily Care: How Do I Protect My Dialysis Access?
Daily care is critical for keeping your access healthy.
DO:
- Keep the area clean
- Check daily for a vibration ("thrill")
- Check daily for a vibration ("thrill")
- Follow needle rotation techniques (if self-aware)
AVOID:
- Blood pressure measurements on the access arm
- Blood draws or injections in that arm
- Tight clothing or jewellery over the access
- Sleeping on the access arm
Warning Signs: When Should I Contact My Doctor Immediately?
Contact your care team if you notice:
- Loss of thrill or bruit
- Sudden swelling of the arm or hand
- Prolonged bleeding after dialysis
- Fever or chills
- Redness, warmth, or discharge at the site
- Hand pain, numbness, or wounds on the access side
Early action can prevent access failure and serious complications.
Common Dialysis Access Problems
Narrowing (Stenosis)
A narrowing in the blood vessel can reduce flow and cause dialysis machine alarms, prolonged bleeding after needle removal, and poor dialysis clearance.
Blood Clots (Thrombosis)
Clots can block the access completely and require urgent treatment.
Infection
More common with catheters and grafts. Signs include fever or chills during dialysis, and redness, warmth, or discharge at the site.
Aneurysms and Pseudoaneurysms
Bulging of the vessel wall due to repeated needle use or high pressure. These require monitoring and sometimes repair.
What Is Steal Syndrome?
Steal syndrome is a condition where too much blood is diverted through the dialysis access, reducing blood flow to the hand or fingers.
Symptoms May Include:
- Coldness in the hand
- Coldness in the hand
- Numbness or tingling
- Weakness
- Pain that worsens during dialysis
- Non-healing wounds or ulcers on fingers (in severe cases)
Why It Happens: The access "steals" blood from the smaller arteries that supply the hand.
What To Do: Steal syndrome should never be ignored. If symptoms occur, prompt evaluation is essential. Treatments are available to restore circulation while preserving the access.
How Is My Dialysis Access Monitored?
Your access should be checked regularly by your dialysis and vascular care team.
Monitoring may include:
- Physical examination (listening for bruit, feeling thrill)
- Measuring blood flow and pressure
- Duplex ultrasound to assess vessel health
Regular monitoring helps detect problems early — often before dialysis efficiency declines.
Who Manages My Dialysis Access?
Surgery and Maintenance:Vascular surgeons or interventional specialists with expertise in blood vessel care create and maintain dialysis access. They also manage access-related complications and perform minimally invasive procedures to restore or preserve access function.
Ongoing Monitoring:Your dialysis team, nephrologist, and vascular or interventional specialist work together to monitor and maintain access health.
RIVEA: Specialized Vascular Care for Dialysis Access
RIVEA is an award-winning single-specialty vascular and endovascular centre, focused entirely on blood vessel health. Dialysis access care is approached as a specialized vascular service, allowing for better expertise, advanced imaging, and comprehensive access management.
Key strengths include:
- Expertise in planning, creation, and maintenance of dialysis access
- Emphasis on minimally invasive, image-guided treatments to preserve access
- Care led by American Board–certified vascular specialists, trained to international standards
- A patient-centric approach that prioritizes safety, comfort, and long-term outcomes
By combining advanced technology with specialised vascular knowledge, RIVEA helps patients maintain reliable dialysis access and avoid unnecessary complications.
FAQs
Why do I need dialysis access before starting dialysis?
Access needs time to heal and mature. Planning early reduces emergency catheter use and complications.
Can my access stop working?
Yes. Access can narrow, clot, or become infected. Regular monitoring helps prevent sudden failure.
What should I do if I can't feel the "thrill"?
Loss of thrill may indicate blockage or clotting. Seek medical attention immediately.
Should blood pressure be measured on the access arm?
No. Blood pressure cuffs can damage the access and should always be avoided on that arm.
Is everyone suitable for an AV fistula?
No. Some patients have veins that are too small or damaged. In such cases, a graft or alternative access is recommended.
Can dialysis access be repaired if it fails?
Yes. Many accesses can be restored using minimally invasive procedures or surgical revision.
What are the most common problems with fistulas and grafts?
Narrowing (stenosis), clotting, infection, and aneurysms or pseudoaneurysms.
What are the long-term complications of dialysis catheters?
Bloodstream infections, vein narrowing, and poor dialysis efficiency. For this reason, catheters are considered temporary.
What should I do if my access is swollen or has an aneurysm?
Avoid cannulating swollen or bulging areas and contact your vascular care team for evaluation.
When should I contact a doctor after access surgery?
Contact your doctor if you experience severe pain, increasing swelling, redness or discharge, fever, or loss of thrill.